Introduction
Blood clots are a serious medical concern that can lead to life-threatening conditions. Their prevention is crucial to avoid complications and maintain overall wellness. Fortunately, Blood Thinners pills offer an effective means to reduce the risk of clot formation and potentially save lives.
The importance of preventing blood clots
Overview of blood thinner pills as a potential solution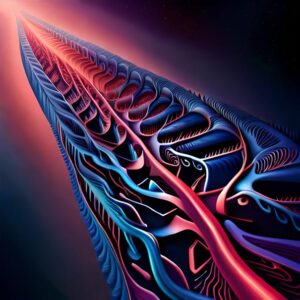
Understanding Blood Clots
Definition and types of blood clots
Risk factors and common health conditions associated with clots
Potential consequences and complications of blood clots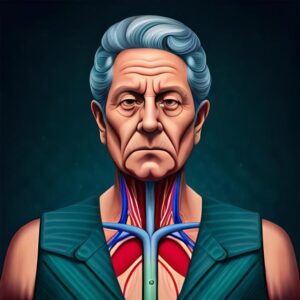
To grasp the significance of blood thinner pills, it is essential to understand what blood clots are, their different types, and the implications they can have on one’s health. Blood clots, also known as thrombi, are gel-like masses that form when blood platelets and proteins known as fibrin become too sticky. These clots can occur in various areas of the body, such as veins, arteries, and even the heart.
Certain risk factors make individuals more susceptible to blood clot formation. These include prolonged immobilization, genetic predisposition, obesity, certain medications, and underlying health conditions such as cancer or diabetes. Blood clots can lead to serious complications, including pulmonary embolism (clots in the lungs), deep vein thrombosis (clots in deep veins, often in the legs), stroke, or heart attack.
Mechanism of Blood Thinners
How blood thinning medications work
Different types of blood thinner pills and their efficacy
Advantages and limitations of blood thinners
Blood thinning medications, commonly referred to as anticoagulants, work by inhibiting the clotting process in the body. They interfere with the chemicals involved in clot formation, preventing the accumulation of platelets and the production of fibrin. This helps to maintain blood flow and reduce the risk of clot formation.
There are various types of blood thinner pills available, each with its own mechanism of action and efficacy. Some commonly prescribed blood thinners include warfarin, heparin, and direct oral anticoagulants (DOACs) such as apixaban and rivaroxaban. These medications have been extensively studied and proven to significantly reduce the occurrence of blood clots.
While blood thinners offer significant benefits in preventing clots, they also have limitations. One of the main concerns is the potential for excessive bleeding as a side effect. However, healthcare providers closely monitor patients to minimize these risks and ensure safe usage of blood thinners.
Conditions that Require Blood Thinners
Venous thromboembolism and deep vein thrombosis
Atrial fibrillation and stroke prevention
Coronary artery disease and heart attack prevention
Blood thinners are essential in managing and preventing various medical conditions that are associated with an increased risk of blood clots. Venous thromboembolism, which encompasses deep vein thrombosis and pulmonary embolism, requires blood thinners to prevent or treat these potentially life-threatening conditions.
Individuals with atrial fibrillation, a heart rhythm disorder, are at a higher risk of stroke due to blood clots forming in the heart. Blood thinners are prescribed to prevent the formation and migration of these clots, reducing the likelihood of a stroke.
Similarly, individuals with coronary artery disease, characterized by the buildup of plaque in the arteries supplying the heart, benefit from blood thinners to prevent the formation of clots that can lead to heart attacks.
Blood Thinners vs. Alternative Treatments
Comparison of blood thinner pills with surgical clot removal
Contrast blood thinners with antiplatelet drugs
Evaluation of blood thinners against lifestyle changes and diet modifications
When considering treatment options for blood clots, it is important to weigh the benefits and drawbacks of blood thinners against alternative approaches. Surgical clot removal, while effective in some cases, involves invasive procedures and carries its own set of risks.
Another class of medications known as antiplatelet drugs, such as apixaban and clopidogrel, can reduce clot formation by inhibiting platelet activation. However, these drugs differ from blood thinners in their mechanism of action and target patient populations.
Moreover, lifestyle changes and dietary modifications can play a significant role in reducing clot formation. While these interventions are important, they often need to be complemented with blood thinners, particularly in individuals with underlying medical conditions or inherited clotting disorders.
Adverse Effects and Management
The risk of excessive bleeding with blood thinners
Monitoring and managing bleeding complications
Methods to reverse the effects of blood thinners in emergencies
The risk of excessive bleeding is a primary concern when using blood thinners. While these medications reduce the likelihood of clot formation, they also interfere with the normal clotting process, increasing the potential for bleeding. However, healthcare providers closely monitor patients on blood thinners and assess their bleeding risk to mitigate potential complications.
In case of bleeding emergencies or the need for urgent surgery, measures exist to reverse the effects of blood thinners. Depending on the situation, healthcare professionals may administer specific medications or use techniques to accelerate the clotting process and control bleeding effectively.
Frequently Asked Questions
- How long do blood thinners need to be taken?
- Are blood thinner injections more effective than pills?
- Can blood thinners dissolve existing clots?
- What happens if a dose of blood thinners is missed?
- How often do blood thinner dosages need adjustment?
- Are there non-prescription alternatives to blood thinning pills?
To address common inquiries, here are answers to some frequently asked questions about blood thinners.
- The duration of blood thinner use varies depending on the individual’s underlying condition and treatment goals.
- Blood thinner injections and pills can be equally effective in preventing blood clots, but the choice of administration depends on the specific circumstances and patient factors.
- Blood thinners do not dissolve existing clots but help prevent the formation of new ones and reduce the risk of clot-related complications.
- If a dose of blood thinner is missed, it is important to consult with a healthcare provider to determine the appropriate course of action.
- Dosage adjustment for blood thinner is done based on individual response and specific health conditions. Regular monitoring and adjustments are made as necessary.
- Non-prescription alternatives to blood thinning pills are limited. It is recommended to consult with a healthcare provider for appropriate treatment options.
Conclusion
Recap of the importance of blood thinner pills in preventing life-threatening clots
Hope for continued advancements in blood-thinning medications
Encouragement for individuals at risk to consult healthcare professionals for guidance
Blood thinner pills play a vital role in preventing life-threatening blood clots, reducing the risk of complications such as stroke, pulmonary embolism, and heart attack. With ongoing research and advancements in blood-thinning medications, there is hope for even more effective and safe treatment options in the future.
Individuals at risk of blood clots are encouraged to seek guidance from healthcare professionals. They can provide tailored treatment plans, ensure proper medication management, and address any concerns or questions regarding blood thinner usage. By working together, healthcare providers and patients can make informed decisions and promote optimal health outcomes.


